Discovering a bump on your knuckle bone can be concerning, especially when it appears seemingly out of nowhere or gradually develops over time. These protrusions, medically termed as osseous prominences or bony enlargements, can arise from numerous underlying conditions ranging from minor trauma to complex systemic diseases. The metacarpophalangeal joints, commonly known as knuckles, are particularly susceptible to various pathological processes due to their frequent use and exposure to mechanical stress. Understanding the diverse aetiological factors behind knuckle bone bumps is crucial for proper diagnosis and treatment, as some conditions require immediate medical attention whilst others may resolve spontaneously.
Traumatic knuckle bone injuries and resulting bumps
Trauma represents one of the most frequent causes of knuckle bone abnormalities, with injuries ranging from acute fractures to chronic overuse conditions. The knuckles, being prominent anatomical structures, are particularly vulnerable to direct impact injuries, falls, and repetitive microtrauma. When the delicate balance of bone formation and resorption is disrupted by trauma, the body’s natural healing response can result in excess bone formation, creating visible bumps or deformities.
Boxer’s fracture of the fifth metacarpal neck
The boxer’s fracture, affecting the neck of the fifth metacarpal bone, commonly occurs when individuals punch hard surfaces with a closed fist. This injury mechanism typically results from striking walls, doors, or other solid objects during moments of anger or frustration. The fracture site often heals with angulation and subsequent callus formation, creating a noticeable bump over the affected knuckle. Improper healing can lead to permanent deformity, with the metacarpal head appearing more prominent than its unaffected counterparts.
Treatment outcomes vary significantly depending on the degree of angulation and whether proper medical intervention was sought initially. Early recognition and appropriate immobilisation can prevent many of the long-term complications associated with this injury. However, when left untreated or inadequately managed, the healing process may result in excessive bone formation and a persistent knuckle prominence that can affect both function and aesthetics.
Metacarpophalangeal joint dislocation complications
Joint dislocations at the metacarpophalangeal level can cause significant structural damage to the surrounding soft tissues and joint capsule. Following reduction of the dislocation, the healing process may involve formation of heterotopic ossification or bone spurs around the joint margins. These bony proliferations manifest as firm bumps that can be palpated around the affected knuckle joint.
The development of post-traumatic arthritis following joint dislocation often contributes to ongoing bone formation irregularities. Patients frequently report persistent swelling and bumpiness around previously dislocated joints, even years after the initial injury. The severity of these changes correlates with the extent of initial soft tissue damage and the adequacy of post-injury rehabilitation.
Chronic repetitive stress fractures in knuckle bones
Repetitive stress injuries of the metacarpal bones can occur in individuals engaged in activities requiring frequent punching motions or repetitive gripping actions. Martial artists, boxers, and manual labourers are particularly susceptible to developing stress fractures that may not be immediately apparent. These microscopic fractures trigger a continuous cycle of bone breakdown and reformation, often resulting in localised bone thickening and knuckle prominence.
The cumulative effect of repeated microtrauma can be more significant than single acute injuries in terms of long-term bone changes. Athletes who ignore early warning signs of stress injuries may develop permanent structural alterations that manifest as visible knuckle bumps. Early recognition of repetitive stress patterns and appropriate activity modification can prevent many of these chronic changes.
Post-traumatic osteophyte formation
Following any significant trauma to the knuckle joints, the development of osteophytes or bone spurs represents a common long-term complication. These bony outgrowths form as part of the body’s attempt to stabilise damaged joint surfaces and can create noticeable bumps around the affected joints. The formation process typically occurs gradually over months to years following the initial injury.
Post-traumatic osteophytes differ from those associated with primary osteoarthritis in their distribution pattern and morphology. They tend to be more irregular in shape and may cause more significant functional impairment due to their location relative to important anatomical structures. The prevention of excessive osteophyte formation relies heavily on proper acute injury management and early mobilisation when appropriate.
Arthritic conditions affecting knuckle bone morphology
Arthritis represents a major category of conditions that can significantly alter knuckle bone architecture, leading to various forms of bony prominences and deformities. The inflammatory processes associated with different types of arthritis trigger complex cascades of bone formation and destruction, often resulting in characteristic patterns of joint changes that can be diagnostic of specific conditions.
Osteoarthritic osteophyte development in MCP joints
Osteoarthritis affecting the metacarpophalangeal joints typically manifests as marginal osteophyte formation, which creates visible and palpable bumps around the joint margins. These bony outgrowths develop as a response to chronic mechanical stress and cartilage degradation, representing the body’s attempt to increase joint surface area and distribute forces more effectively. The osteophytes commonly form on the dorsal and lateral aspects of the metacarpal heads, creating characteristic knuckle enlargement.
The progression of osteoarthritic changes in the knuckles follows a predictable pattern, beginning with subtle joint space narrowing and progressing to more obvious osteophyte formation. Early-stage disease may be asymptomatic , with patients first noticing cosmetic changes before experiencing functional limitations. The rate of progression varies considerably between individuals, influenced by factors such as occupational demands, genetic predisposition, and previous joint injuries.
Rheumatoid arthritis nodule formation
Rheumatoid nodules represent a characteristic extra-articular manifestation of rheumatoid arthritis, commonly developing over pressure points including the knuckle areas. These firm, usually painless subcutaneous masses can vary significantly in size and may fluctuate in prominence over time in correlation with disease activity. Unlike bony prominences, rheumatoid nodules are composed of granulomatous tissue and can occasionally ulcerate or become infected.
The development of rheumatoid nodules correlates strongly with the presence of rheumatoid factor and anti-cyclic citrullinated peptide antibodies in the patient’s serum.
Approximately 20-30% of patients with rheumatoid arthritis develop subcutaneous nodules during the course of their disease, with the knuckle area being one of the most common locations.
The nodules may precede joint symptoms in some cases, making them an important early diagnostic clue.
Psoriatic arthritis bone proliferation patterns
Psoriatic arthritis demonstrates unique patterns of bone formation that can create distinctive knuckle abnormalities, particularly in patients with the arthritis mutilans subtype. The condition is characterised by both bone formation and destruction occurring simultaneously, leading to irregular joint contours and asymmetric knuckle enlargement. The “pencil-in-cup” deformity represents an extreme example of these changes, where bone destruction and proliferation create characteristic radiographic appearances.
Unlike rheumatoid arthritis, psoriatic arthritis tends to affect joints asymmetrically and may spare certain areas whilst severely affecting others. The bone proliferation associated with this condition often creates more irregular and unpredictable knuckle changes compared to the more uniform osteophyte formation seen in osteoarthritis. Early diagnosis and treatment with disease-modifying agents can significantly alter the natural progression of these bone changes.
Gouty tophi deposits on metacarpal heads
Chronic gout can result in the formation of tophi, which are deposits of monosodium urate crystals that can accumulate in and around the knuckle joints. These deposits create firm, sometimes ulcerating nodules that can be mistaken for other types of knuckle bumps. Tophi typically develop in patients with longstanding, inadequately treated hyperuricaemia and represent a sign of advanced gouty arthritis.
The location of gouty tophi around the knuckles often correlates with areas of previous acute gouty attacks, suggesting that local tissue damage may predispose to crystal deposition. The tophi can cause significant cosmetic concerns and may interfere with normal hand function when they become large enough to impede joint movement. Modern urate-lowering therapies can lead to gradual dissolution of tophi over time, making early recognition and treatment paramount.
Benign bone tumours and cystic lesions
Benign bone tumours and cystic lesions affecting the metacarpal bones, whilst less common than traumatic or arthritic causes, can create significant knuckle prominences that may be concerning to patients. These lesions often present as slowly growing masses that may or may not be associated with pain, and their benign nature can only be confirmed through appropriate imaging studies and sometimes tissue sampling.
Enchondroma formation in metacarpal bones
Enchondromas represent the most common primary bone tumour affecting the small bones of the hand, including the metacarpals. These benign cartilaginous lesions typically develop within the medullary cavity and can cause localised expansion of the bone, creating a palpable bump over the affected knuckle area. Most enchondromas are asymptomatic and discovered incidentally on radiographs obtained for other reasons.
The clinical significance of enchondromas lies in their potential for pathological fracture, particularly when they reach significant size or when located in weight-bearing areas of the metacarpal. Multiple enchondromas may suggest underlying conditions such as Ollier disease or Maffucci syndrome, which require different management approaches. The malignant transformation risk of solitary enchondromas in the hand is extremely low, but any change in size or symptoms warrants immediate evaluation.
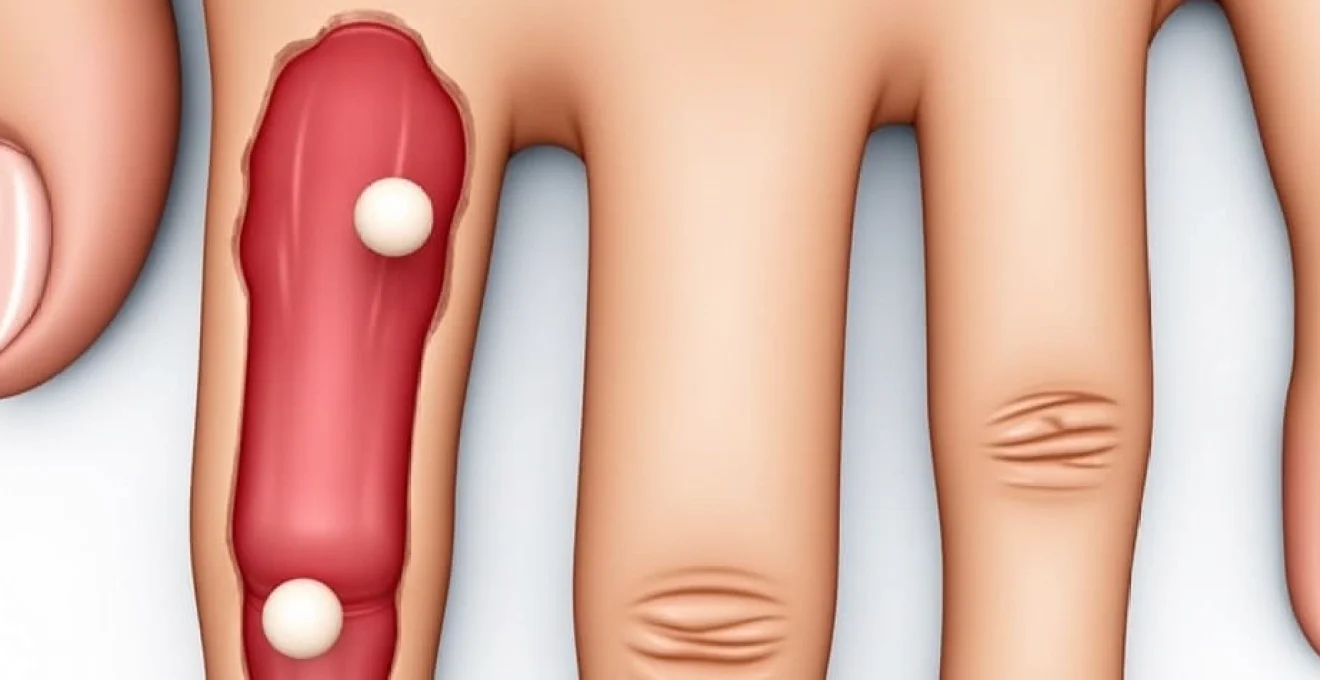
Giant cell tumour of tendon sheath manifestations
Giant cell tumours of the tendon sheath commonly affect the fingers and can create masses that appear to arise from the knuckle area when they involve the flexor or extensor tendons crossing the metacarpophalangeal joints. These benign soft tissue tumours are the second most common tumour affecting the hand and typically present as slowly growing, painless masses that may interfere with normal finger function.
The tumours characteristically demonstrate a lobulated appearance and may appear to fluctuate in size with finger movement due to their relationship with the surrounding tendon structures.
Giant cell tumours of the tendon sheath have a tendency to recur if incompletely excised, making thorough surgical removal essential for definitive treatment.
The proximity to important neurovascular structures often makes surgical planning challenging, requiring expertise in hand surgery techniques.
Ganglion cyst development adjacent to knuckle joints
Ganglion cysts arising from or adjacent to the metacarpophalangeal joints can create bump-like protrusions that patients may interpret as knuckle bone abnormalities. These fluid-filled sacs typically originate from joint capsules or tendon sheaths and contain thick, jelly-like synovial fluid. The cysts may fluctuate in size and can sometimes be transilluminated to confirm their fluid-filled nature.
Dorsal ganglion cysts of the hand often arise from the scapholunate ligament area but can extend distally to create prominence near the knuckle region. The characteristic features include their smooth, rounded contour and the ability to move them relative to surrounding structures. Aspiration of ganglion cysts can provide temporary relief but has high recurrence rates, making surgical excision the preferred definitive treatment for symptomatic lesions.
Epidermoid cyst formation over metacarpal heads
Epidermoid cysts, also known as sebaceous or inclusion cysts, can develop over the knuckle area following minor trauma or embedded foreign bodies. These cysts form when surface epithelium becomes trapped beneath the skin surface, creating a keratin-filled cavity that gradually enlarges over time. The cysts typically present as smooth, moveable masses that may have a central punctum or opening.
The formation of epidermoid cysts over the knuckles often follows penetrating injuries such as glass cuts or splinter wounds, where epithelial cells are driven into deeper tissues. The cysts may remain stable for years before becoming symptomatic due to secondary infection or rapid growth. Surgical excision with complete removal of the cyst wall is necessary to prevent recurrence and address any associated complications.
Infectious osteomyelitis and septic arthritis sequelae
Infectious processes affecting the knuckle bones and joints can result in significant structural changes that manifest as bony prominences or irregular joint contours. Both acute and chronic infections can trigger inflammatory responses that lead to bone formation irregularities, joint destruction, and subsequent healing with deformity. The metacarpophalangeal joints are particularly susceptible to infection following penetrating injuries, animal bites, or as a complication of systemic bacteraemia.
Chronic osteomyelitis of the metacarpal bones often results in irregular bone formation as the body attempts to wall off infected areas through sclerotic bone formation and involucrum development. This process can create significant bony prominences that may persist long after the acute infection has resolved. The sequela of chronic osteomyelitis frequently includes areas of bone death (sequestra) surrounded by reactive new bone formation, leading to an irregular, bumpy appearance of the affected knuckle area.
Septic arthritis of the metacarpophalangeal joints, if not promptly and adequately treated, can result in joint space narrowing, ankylosis, and irregular periarticular bone formation. The inflammatory mediators released during bacterial joint infection can stimulate osteoblast activity whilst simultaneously promoting bone resorption, leading to complex patterns of bone formation and destruction. Patients with a history of septic arthritis may develop chronic joint deformities that include bony prominences around the previously infected joint.
Post-infectious joint changes often include the formation of bone spurs and irregular joint margins as the body attempts to restore joint stability following cartilage destruction. These changes can create permanent knuckle enlargement and functional impairment that may require surgical intervention to restore acceptable function and appearance. Early recognition and aggressive treatment of hand infections are crucial for preventing these long-term complications that can significantly impact hand function and quality of life.
Congenital anomalies and developmental disorders
Congenital abnormalities affecting knuckle bone development can manifest as various forms of bony prominences or irregular joint architecture that become apparent during childhood or adolescence. These developmental anomalies may result from genetic mutations, intrauterine environmental factors, or disruptions in normal embryological development processes. Understanding these conditions is crucial for appropriate management and counselling of affected individuals and their families.
Metacarpal coalition or fusion abnormalities can create unusual knuckle contours that may be mistaken for acquired conditions. These developmental anomalies typically involve abnormal connections between adjacent bones or incomplete separation of structures that should normally be distinct.
Congenital hand anomalies occur in approximately 1 in every 600-700 live births, with many involving the metacarpal and digital structures that can affect knuckle appearance and function.
The timing of recognition often depends on the severity of the abnormality and its impact on hand function.
Developmental disorders such as multiple hereditary exostoses can affect the metacarpal bones, creating characteristic bony outgrowths that may be apparent around the knuckle areas. These benign bone tumours typically develop during periods of rapid skeletal growth and may continue to enlarge until skeletal maturity is reached. The exostoses can create significant cosmetic concerns and may interfere with normal hand function if they impinge on surrounding soft tissues or adjacent bones.
Early recognition of congenital hand anomalies allows for appropriate family counselling and planning of reconstructive procedures when indicated. Many of these conditions have genetic components that may affect family planning decisions and require ongoing monitoring for potential complications or malignant transformation in certain cases. The multidisciplinary approach involving hand surgeons, geneticists, and occupational therapists often provides the best outcomes for patients with complex congenital hand conditions affecting knuckle structure and function.
Diagnostic imaging protocols for knuckle bone abnormalities
Accurate diagnosis of knuckle bone bumps requires systematic evaluation using appropriate imaging modalities, each offering unique advantages in
visualising soft tissue structures and bone details respectively. Plain radiography remains the initial imaging study of choice for evaluating knuckle bone abnormalities, providing excellent detail of bone architecture, joint spaces, and calcified structures. Standard posteroanterior and lateral views of the hand can reveal fractures, arthritis changes, bone tumours, and other osseous abnormalities that may manifest as knuckle bumps.
Advanced cross-sectional imaging techniques offer superior soft tissue contrast and multiplanar reconstruction capabilities that enhance diagnostic accuracy. Magnetic resonance imaging excels in evaluating soft tissue masses, joint effusions, cartilage integrity, and bone marrow changes that may not be apparent on conventional radiographs. The ability to differentiate between various tissue types makes MRI particularly valuable for distinguishing between solid tumours, cystic lesions, and inflammatory conditions affecting the knuckle region.
Ultrasound imaging has emerged as a valuable tool for evaluating superficial masses and can effectively differentiate between solid and cystic lesions adjacent to the knuckle joints. The real-time nature of ultrasound examination allows for dynamic assessment of lesion mobility and relationship to surrounding structures. High-frequency transducers can provide excellent resolution of superficial soft tissue abnormalities, making ultrasound an ideal first-line imaging modality for evaluating suspected ganglion cysts, lipomas, and other soft tissue masses.
Computed tomography scanning offers superior bone detail compared to conventional radiography and can reveal subtle fractures, bone tumours, and complex joint abnormalities that may be overlooked on plain films.
CT imaging with three-dimensional reconstruction capabilities can provide crucial information for surgical planning, particularly in cases involving complex fractures or bone tumours requiring precise localisation.
The use of contrast enhancement in CT studies can help differentiate between vascular and avascular lesions, providing additional diagnostic information that influences treatment decisions.
Specialised imaging techniques such as bone scintigraphy may be indicated in cases where infection, malignancy, or metabolic bone disease is suspected. Nuclear medicine studies can detect areas of increased bone turnover that may not be apparent on anatomical imaging studies, making them valuable for early detection of osteomyelitis or metastatic disease affecting the metacarpal bones. The high sensitivity of bone scans makes them particularly useful for screening multiple skeletal sites when systemic conditions are suspected as the underlying cause of knuckle bone abnormalities.
Proper imaging protocol selection requires consideration of the clinical presentation, duration of symptoms, and suspected underlying pathology. A systematic approach to imaging evaluation ensures that appropriate studies are performed in a cost-effective manner whilst maximising diagnostic yield. The integration of clinical findings with imaging results forms the foundation for accurate diagnosis and appropriate treatment planning for patients presenting with knuckle bone bumps and associated symptoms.