Eustachian tube dysfunction (ETD) affects millions of patients worldwide, presenting as ear pressure, hearing difficulties, and recurrent infections that significantly impact quality of life. While various treatment modalities exist, prednisolone has emerged as a valuable therapeutic option for managing this challenging condition. The use of oral corticosteroids in ETD treatment represents a targeted approach to addressing the underlying inflammatory processes that contribute to tube dysfunction and associated symptoms.
The complexity of ETD pathophysiology requires a nuanced understanding of how systemic corticosteroids like prednisolone can effectively modulate the inflammatory cascade within the upper respiratory tract. Current evidence suggests that short-term prednisolone therapy can provide rapid symptom relief, though the long-term benefits remain limited. This therapeutic approach becomes particularly relevant when considering the significant impact ETD has on patient wellbeing and the need for effective non-surgical interventions.
Eustachian tube dysfunction pathophysiology and clinical presentation
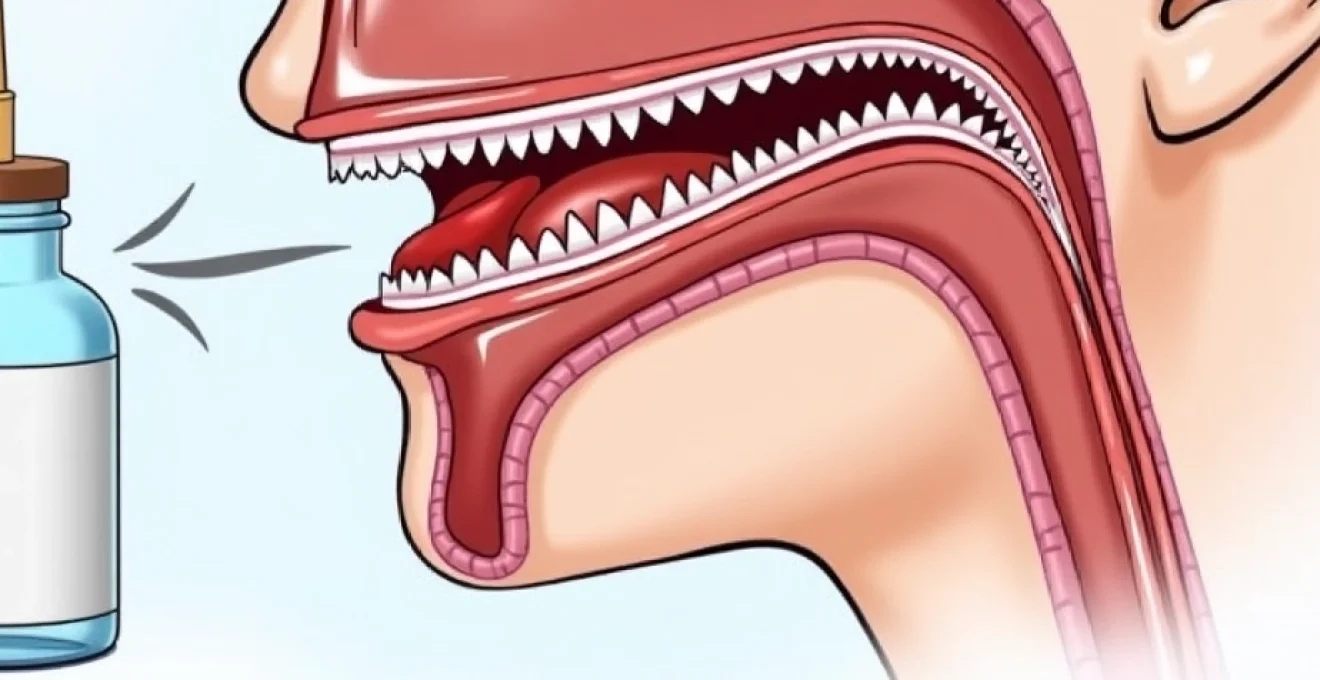
The eustachian tube serves as a critical anatomical bridge connecting the middle ear to the nasopharynx, facilitating pressure equalisation and drainage of secretions. When this tube fails to function properly, patients experience a constellation of symptoms that can severely affect their daily activities. Understanding the underlying mechanisms of ETD provides essential context for evaluating prednisolone’s therapeutic role in treatment protocols.
ETD encompasses both obstructive and patulous forms, with the obstructive type being more commonly encountered in clinical practice. The condition often develops secondary to upper respiratory tract infections, allergic rhinitis, or chronic sinusitis, creating a cascade of inflammatory responses that impair normal tube function. Patients typically present with subjective hearing loss , ear fullness, and difficulty equalising pressure during altitude changes.
Mucosal inflammation and ciliary dysfunction in ETD pathogenesis
The pathogenesis of ETD primarily involves inflammatory changes within the tubal mucosa, leading to oedema and impaired ciliary function. Inflammatory mediators such as histamine, leukotrienes, and prostaglandins contribute to mucosal swelling and increased secretion production. This inflammatory process disrupts the normal ciliary transport mechanism, resulting in accumulation of secretions and further tube obstruction.
Chronic inflammation can lead to structural changes within the eustachian tube, including mucosal thickening and fibrosis. These alterations perpetuate the dysfunction and make the condition more resistant to conservative treatment measures. The inflammatory environment also promotes bacterial colonisation, potentially leading to recurrent otitis media and further complications.
Barotrauma-induced eustachian tube obstruction mechanisms
Barotrauma represents a significant trigger for acute ETD, particularly in individuals with pre-existing tube dysfunction. Rapid pressure changes during air travel or diving can overwhelm the tube’s compensatory mechanisms, leading to acute obstruction and severe symptoms. The inability to equalise pressure effectively can result in tympanic membrane retraction or even perforation in severe cases.
The physiological response to barotrauma involves reflexive muscle contraction and inflammatory changes that further compromise tube patency. Patients experiencing barotrauma-induced ETD often require immediate intervention to prevent complications such as hearing loss or secondary infection. Prednisolone’s anti-inflammatory properties make it particularly valuable in these acute scenarios where rapid symptom resolution is essential.
Allergic rhinitis and ETD symptom correlation studies
Research has consistently demonstrated a strong correlation between allergic rhinitis and ETD development, with studies showing that approximately 40-60% of patients with chronic ETD have concurrent allergic disease. The allergic inflammatory cascade involving mast cell degranulation and eosinophil recruitment directly affects eustachian tube mucosa, leading to oedema and dysfunction.
Seasonal variations in ETD symptoms often mirror allergic rhinitis patterns, suggesting shared pathophysiological mechanisms. Patients with allergic ETD frequently experience symptom exacerbations during peak allergen seasons, requiring targeted anti-inflammatory interventions. The systemic nature of allergic inflammation makes oral corticosteroids like prednisolone particularly effective in addressing both nasal and tubal symptoms simultaneously.
Tympanometric findings in chronic eustachian tube dysfunction
Tympanometry provides objective assessment of eustachian tube function and middle ear status in patients with ETD. Characteristic findings include reduced tympanic membrane mobility, negative middle ear pressure, and abnormal pressure-compliance relationships. These measurements help clinicians assess treatment response and guide therapeutic decisions.
Chronic ETD often presents with type B or C tympanograms, indicating either fluid accumulation or negative pressure within the middle ear space. Serial tympanometric assessments can demonstrate improvement in tube function following prednisolone therapy, providing objective evidence of treatment efficacy. However, the correlation between tympanometric improvement and symptom resolution varies among patients, highlighting the importance of comprehensive clinical evaluation.
Prednisolone pharmacodynamics in upper respiratory tract inflammation
Prednisolone’s mechanism of action in treating ETD involves complex interactions at the cellular and molecular level, targeting multiple inflammatory pathways that contribute to tube dysfunction. Understanding these pharmacodynamic principles helps clinicians optimise treatment protocols and predict therapeutic outcomes. The drug’s systemic distribution allows it to reach inflamed tissues throughout the upper respiratory tract, making it particularly effective for conditions involving multiple anatomical sites.
The therapeutic window for prednisolone in ETD treatment typically involves short-term, high-dose administration to achieve rapid anti-inflammatory effects whilst minimising systemic side effects. This approach capitalises on the drug’s ability to suppress acute inflammatory responses without causing significant hypothalamic-pituitary-adrenal axis suppression. Clinical studies have demonstrated that even brief courses of prednisolone can provide meaningful symptom improvement in selected patients with ETD.
Glucocorticoid receptor binding and Anti-Inflammatory cascade
Prednisolone exerts its anti-inflammatory effects through binding to cytoplasmic glucocorticoid receptors, forming complexes that translocate to the nucleus and modulate gene transcription. This genomic mechanism leads to increased production of anti-inflammatory proteins whilst suppressing pro-inflammatory mediators. The process typically requires several hours to initiate, explaining why patients may not experience immediate symptom relief following oral administration.
The drug’s ability to suppress nuclear factor-kappa B (NF-κB) activation plays a crucial role in reducing inflammatory cytokine production within the eustachian tube mucosa. This suppression leads to decreased production of interleukin-1β, tumour necrosis factor-α, and other inflammatory mediators that contribute to mucosal oedema and dysfunction. The genomic effects of prednisolone provide sustained anti-inflammatory activity that can persist beyond the drug’s plasma half-life.
Mucosal oedema reduction through Prednisolone-Mediated vasoconstriction
Beyond its genomic effects, prednisolone also exerts rapid non-genomic actions that contribute to its therapeutic efficacy in ETD. These include membrane stabilisation effects and modulation of calcium influx, leading to reduced vascular permeability and oedema formation. The vasoconstrictor effects help restore normal mucosal thickness within the eustachian tube, improving patency and function.
The reduction in mucosal oedema occurs through multiple mechanisms, including decreased capillary permeability and enhanced lymphatic drainage. Clinical studies have shown that patients often experience symptom improvement within 24-48 hours of initiating prednisolone therapy, suggesting that both genomic and non-genomic mechanisms contribute to therapeutic efficacy. This dual action profile makes prednisolone particularly valuable for acute ETD presentations requiring rapid intervention.
Cytokine suppression effects on eustachian tube epithelium
Prednisolone’s immunosuppressive effects extend to modulation of cytokine networks within the eustachian tube epithelium, creating an environment more conducive to normal physiological function. The drug suppresses production of pro-inflammatory cytokines such as interleukin-6, interleukin-8, and granulocyte-macrophage colony-stimulating factor, all of which contribute to ETD pathogenesis.
The restoration of normal cytokine balance helps re-establish proper ciliary function and mucociliary clearance within the eustachian tube. This improvement in clearance mechanisms reduces the likelihood of secondary bacterial infections and promotes resolution of accumulated secretions. Research has demonstrated that prednisolone therapy can normalise epithelial cell function markers within days of treatment initiation.
Pharmacokinetic profile of oral prednisolone in otolaryngological applications
The pharmacokinetic properties of oral prednisolone make it well-suited for ETD treatment, with rapid absorption and distribution to target tissues throughout the upper respiratory tract. Peak plasma concentrations typically occur within 1-2 hours of oral administration, with therapeutic levels maintained for 12-36 hours depending on the dose administered. This pharmacokinetic profile allows for once-daily dosing in most clinical scenarios.
The drug’s hepatic metabolism through 11β-hydroxysteroid dehydrogenase produces both active and inactive metabolites, with the active form (prednisolone) being responsible for therapeutic effects. Individual variations in enzyme activity can affect treatment response, explaining why some patients require dose adjustments to achieve optimal outcomes. Understanding these pharmacokinetic principles helps clinicians develop personalised treatment protocols for patients with ETD.
Clinical evidence for prednisolone treatment in ETD management
The evidence base supporting prednisolone use in ETD treatment derives primarily from studies focusing on otitis media with effusion and associated eustachian tube dysfunction. A comprehensive Cochrane review examining oral corticosteroid therapy included 108 children and demonstrated significant short-term improvements in middle ear effusion resolution. The relative risk of 4.48 (95% confidence interval: 1.52-13.23) indicates substantial therapeutic benefit during the initial treatment period.
However, the evidence also reveals important limitations regarding long-term efficacy. Studies consistently show that whilst prednisolone provides meaningful short-term symptom relief and objective improvements in tympanometry findings, these benefits rarely persist beyond four weeks following treatment completion. This temporal limitation has important implications for treatment planning and patient counselling regarding realistic expectations.
Clinical trials demonstrate that oral corticosteroids improve OME resolution rates by nearly 350% compared to placebo during the first month of therapy, though benefits do not persist beyond four weeks.
Research examining combination therapy approaches has yielded mixed results, with some studies showing enhanced efficacy when prednisolone is combined with antibiotics. Five randomised controlled trials involving 409 children found that oral corticosteroids plus antibiotics improved resolution rates with a relative risk of 1.99 (95% CI: 1.14-3.49) compared to placebo plus antibiotic therapy. This suggests potential synergistic effects, particularly in patients with concurrent bacterial infections.
Importantly, studies evaluating hearing outcomes have shown less consistent results, with one trial of 44 children demonstrating no significant improvement in auditory function despite objective improvements in middle ear status. This discordance between objective findings and functional outcomes highlights the complexity of ETD pathophysiology and the need for comprehensive outcome assessments in clinical practice. The disconnect between tympanometric improvements and hearing restoration suggests that structural improvements may not always translate to functional benefits.
Adult studies examining prednisolone efficacy in ETD are more limited but generally consistent with paediatric findings. One randomised controlled trial involving 91 adults with otitis media and effusion found that while corticosteroids improved some objective measures, symptom relief was variable and often temporary. These findings underscore the importance of patient selection and realistic expectation setting when considering prednisolone therapy for adult ETD patients.
Prednisolone dosage protocols and administration guidelines for ETD
Establishing optimal prednisolone dosing regimens for ETD requires careful consideration of multiple factors, including patient age, severity of symptoms, concurrent medications, and individual risk factors for adverse effects. Current evidence supports short-term, high-dose protocols that maximise anti-inflammatory effects whilst minimising the risk of systemic complications. The goal is to achieve rapid symptom resolution whilst avoiding prolonged exposure that could lead to significant side effects.
Clinical practice typically involves initiating therapy with doses equivalent to 1-2 mg/kg/day in children or 40-60 mg daily in adults, administered for 5-14 days depending on symptom severity and treatment response. This approach capitalises on prednisolone’s rapid onset of action whilst limiting exposure duration to reduce the risk of adverse effects. Patient monitoring during treatment helps ensure appropriate response and early detection of potential complications.
Short-term High-Dose prednisolone regimens for acute ETD
Acute ETD presentations, particularly those associated with barotrauma or severe allergic reactions, often benefit from high-dose prednisolone therapy initiated as soon as possible after symptom onset. Typical regimens involve 1-2 mg/kg daily (maximum 80 mg) for children or 60-80 mg daily for adults, administered for 5-7 days. This aggressive approach helps interrupt the inflammatory cascade before permanent structural changes occur.
The rationale for high-dose therapy stems from the need to achieve tissue concentrations sufficient to suppress severe inflammatory responses effectively. Lower doses may prove inadequate in severe cases, leading to treatment failure and potential progression to chronic dysfunction. Clinical experience suggests that early, aggressive intervention often produces superior outcomes compared to conservative approaches in acute presentations.
Tapering schedules to prevent Hypothalamic-Pituitary-Adrenal suppression
For treatment courses exceeding 7-10 days or in patients receiving high-dose therapy, implementing appropriate tapering schedules becomes essential to prevent adrenal insufficiency. Typical tapering involves reducing the daily dose by 25-50% every 3-5 days until discontinuation, though individual patient factors may require modification of this approach. The tapering schedule should be individualised based on treatment duration, initial dose, and patient response.
Patients with concurrent conditions requiring chronic corticosteroid therapy or those with previous exposure to systemic steroids may require more gradual tapering to prevent withdrawal symptoms. Clinical monitoring during the tapering phase helps identify patients who may benefit from slower dose reduction or additional supportive measures. Careful attention to tapering protocols helps minimise the risk of symptom rebound whilst ensuring patient safety.
Paediatric dosing considerations for ETD-Related prednisolone therapy
Paediatric patients present unique considerations for prednisolone dosing, including concerns about growth suppression, behavioural changes, and increased susceptibility to infections. Weight-based dosing typically involves 1-2 mg/kg/day, with maximum daily doses rarely exceeding 60 mg regardless of weight. Treatment duration in children should generally be limited to 5-10 days unless exceptional circumstances warrant longer therapy.
Parents require comprehensive education about potential side effects, including mood changes, increased appetite, and sleep disturbances that commonly occur during treatment. Monitoring growth velocity becomes important if repeated courses are necessary, as even short-term therapy can temporarily affect growth patterns. The benefits of treatment must be carefully weighed against these potential risks in each individual case.
Combination therapy with nasal corticosteroids and oral prednisolone
The concurrent use of intranasal corticosteroids with oral prednisolone therapy represents a logical approach to maximising topical anti-inflammatory effects whilst minimising systemic exposure duration. This combination strategy allows for transition to topical maintenance therapy as oral prednisolone is tapered, potentially extending therapeutic benefits beyond the typical four-week window observed with oral therapy alone.
Evidence supporting combination therapy remains limited, but clinical experience suggests potential benefits in selected patients with concurrent allergic rhinitis or chronic sinusitis. The intranasal component helps address underlying allergic inflammation that may perpetuate ETD, whilst oral prednisolone provides rapid systemic effects. This approach requires careful coordination to avoid excessive total corticosteroid exposure and associated side effects.
Contraindications and adverse effects profile in ETD treatment
Whilst prednisolone offers significant therapeutic benefits for ETD management, its use requires careful consideration of contraindications and potential adverse effects that may limit its application in certain patient populations. The drug’s systemic effects extend beyond the intended target tissues, necessitating comprehensive patient evaluation before initiating therapy. Understanding these limitations helps clinicians make informed treatment decisions and implement appropriate monitoring protocols.
Absolute contraindications to prednisolone therapy include systemic fungal infections, hypersensitivity to the medication, and administration of live virus vaccines. Relative contraindications require careful risk-benefit assessment and may include diabetes mell
itus, hypertension, peptic ulcer disease, osteoporosis, psychiatric disorders, and immunocompromised states. These conditions require enhanced monitoring and potentially modified dosing protocols to minimise treatment-related complications.
Common adverse effects of short-term prednisolone therapy include gastrointestinal upset, mood changes, sleep disturbances, and increased appetite. These effects typically resolve within days of treatment completion but can significantly impact patient quality of life during therapy. More serious complications such as hyperglycaemia, hypertension, and increased infection susceptibility require prompt recognition and management.
The risk-benefit profile of prednisolone in ETD treatment generally favours its use in acute presentations where rapid symptom resolution is essential. However, patients with multiple comorbidities or those requiring repeated treatment courses may benefit from alternative therapeutic approaches. Careful patient selection and monitoring protocols help maximise therapeutic benefits whilst minimising potential complications.
Alternative corticosteroid interventions and treatment comparisons
When oral prednisolone is contraindicated or poorly tolerated, several alternative corticosteroid interventions may provide therapeutic benefits for ETD management. Intranasal corticosteroids represent the most commonly employed alternative, offering targeted anti-inflammatory effects with minimal systemic absorption. However, evidence for their efficacy in ETD remains limited, with studies consistently showing minimal benefit compared to placebo treatments.
Topical nasal corticosteroids such as mometasone, fluticasone, and budesonide have been extensively studied in ETD populations, with disappointing results regarding both symptom improvement and objective measures of tube function. A randomised controlled trial involving 200 children treated with daily mometasone found no difference in hearing loss duration compared to placebo after three months of therapy. These findings suggest that topical approaches may be insufficient for addressing the systemic inflammatory processes underlying ETD.
Injectable corticosteroids, including intratympanic administration, represent another alternative approach for selected patients. This method allows for high local concentrations whilst minimising systemic exposure, potentially offering advantages in patients with contraindications to oral therapy. However, the invasive nature of this approach and limited evidence base restrict its use to specialised centres and refractory cases.
Research comparing different corticosteroid delivery methods consistently demonstrates superior efficacy for systemic oral administration compared to topical or injectable approaches in ETD management.
Combination approaches utilising multiple corticosteroid formulations may offer theoretical advantages by addressing both local and systemic inflammatory components simultaneously. Some clinicians advocate for initiating therapy with oral prednisolone followed by maintenance with intranasal steroids, though evidence supporting this strategy remains anecdotal. The complexity of such regimens must be balanced against potential benefits and patient compliance considerations.
Non-corticosteroid anti-inflammatory agents, including leukotriene receptor antagonists such as montelukast, have shown promise in selected patients with allergic ETD. These agents offer different mechanisms of action and may be particularly valuable in patients with concurrent asthma or significant allergic rhinitis. However, their efficacy as monotherapy for ETD appears inferior to systemic corticosteroids based on current evidence.
The development of newer corticosteroid formulations with improved receptor selectivity and reduced systemic effects may offer future alternatives to traditional prednisolone therapy. Research into selective glucocorticoid receptor modulators continues to evolve, potentially providing enhanced therapeutic ratios for inflammatory conditions affecting the upper respiratory tract. These emerging therapeutic options may eventually offer improved outcomes with reduced adverse effect profiles for patients with chronic or recurrent ETD.
When comparing treatment modalities, oral prednisolone consistently demonstrates superior short-term efficacy compared to alternative approaches, though this advantage must be weighed against its systemic side effect profile. The choice between different corticosteroid interventions should be individualised based on patient factors, symptom severity, treatment history, and contraindications. In cases where multiple treatment failures have occurred, consultation with otolaryngology specialists may help identify patients who would benefit from surgical interventions such as eustachian tube balloon dilation or tympanostomy tube placement.
The integration of prednisolone therapy within comprehensive ETD management protocols requires careful consideration of timing, dosing, and monitoring requirements. Successful treatment often involves addressing underlying predisposing factors such as allergic rhinitis, gastroesophageal reflux, or chronic sinusitis alongside anti-inflammatory interventions. This multidisciplinary approach helps optimise outcomes whilst reducing the likelihood of symptom recurrence following corticosteroid discontinuation.