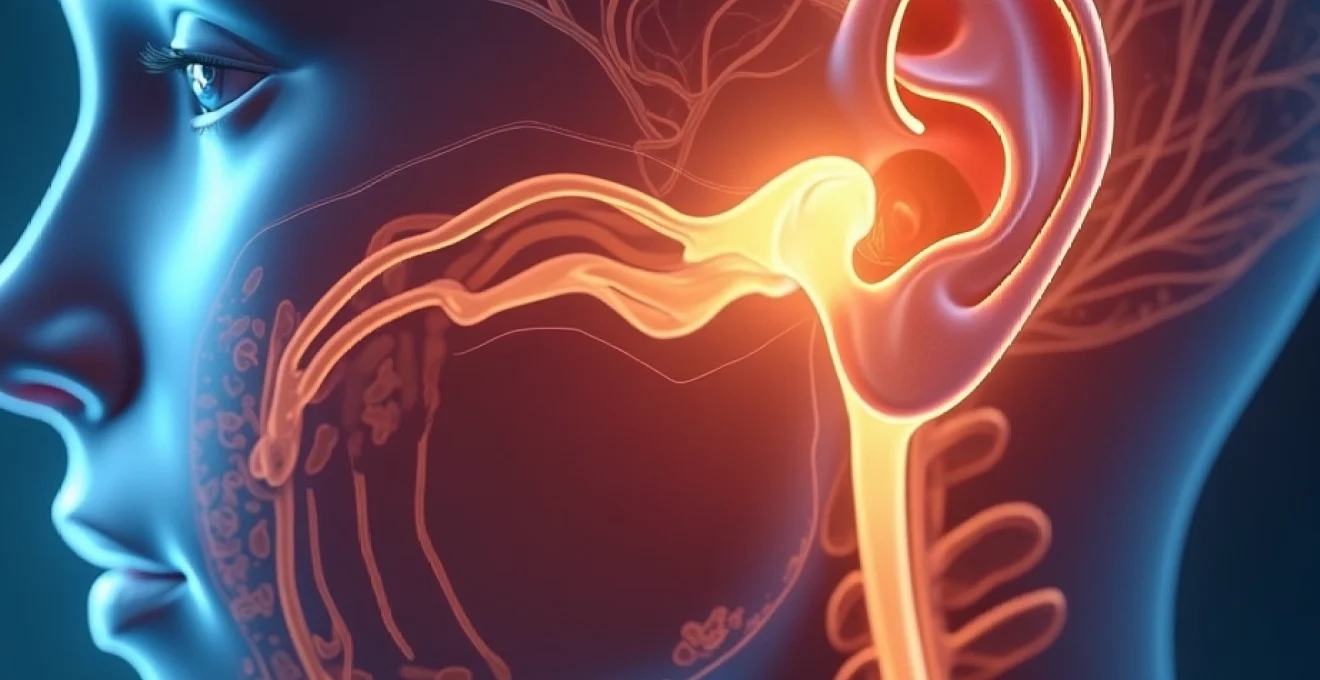
The connection between psychological distress and physical symptoms has become increasingly recognised in modern medicine, with anxiety-induced ear pressure representing a particularly complex manifestation of the mind-body relationship. Millions of individuals worldwide experience unexplained auricular sensations that cannot be attributed to conventional otological pathology, yet significantly impact their quality of life. This phenomenon occurs when the body’s stress response system triggers a cascade of physiological changes that directly affect the delicate structures within the ear, creating sensations of fullness, pressure, and discomfort that can be both distressing and perplexing.
Recent clinical research has demonstrated that anxiety disorders affect approximately 31% of adults at some point in their lives, with a substantial proportion experiencing somatic symptoms including ear-related complaints. The intricate neural pathways connecting the brain’s emotional centres to the auditory and vestibular systems create a complex web of interactions that can produce genuine physical sensations in response to psychological stress. Understanding these mechanisms is crucial for both patients and healthcare providers to develop effective treatment strategies that address the root cause rather than merely managing symptoms.
Neurophysiological mechanisms behind Anxiety-Induced aural pressure
The neurophysiological basis of anxiety-related ear pressure involves multiple interconnected systems working in concert to produce the characteristic sensations experienced by affected individuals. The primary mechanism centres around the dysregulation of the autonomic nervous system, which controls involuntary bodily functions including blood pressure, heart rate, and the delicate pressure balance within the middle ear cavity.
Autonomic nervous system activation and eustachian tube dysfunction
When anxiety triggers the sympathetic nervous system, it initiates a complex sequence of physiological changes that directly impact Eustachian tube function. The sympathetic activation causes vasoconstriction of the small blood vessels supplying the middle ear mucosa, leading to reduced oxygenation and altered cellular metabolism. This vascular compromise affects the normal secretory function of the mucosal lining, potentially causing fluid accumulation and pressure imbalances.
The Eustachian tube muscles, particularly the tensor veli palatini and levator veli palatini, become hyperresponsive during periods of heightened anxiety. Research has shown that chronic stress can lead to sustained muscle tension in these structures, preventing the normal opening and closing mechanism that equalises pressure between the middle ear and the atmosphere. This dysfunction creates the characteristic sensation of fullness and pressure that many anxiety sufferers describe.
Cortisol release and middle ear inflammatory response
The hypothalamic-pituitary-adrenal (HPA) axis activation during anxiety episodes results in elevated cortisol levels, which paradoxically can trigger inflammatory responses in sensitive individuals. Chronic cortisol elevation has been associated with increased permeability of the blood-labyrinthine barrier, allowing inflammatory mediators to enter the inner ear space. This process can contribute to fluid retention and pressure sensations that persist even after the initial anxiety trigger has resolved.
Studies have demonstrated that prolonged stress-hormone exposure can alter the ionic composition of both perilymph and endolymph, the specialized fluids within the inner ear. These compositional changes affect the normal pressure gradients necessary for optimal auditory function and can create sensations of blockage or pressure that patients often struggle to describe accurately to healthcare providers.
Sympathetic overstimulation and tensor tympani muscle contraction
The tensor tympani muscle, located within the middle ear, plays a crucial role in protecting the ear from loud sounds and maintaining optimal hearing sensitivity. During anxiety episodes, sympathetic overstimulation can cause this muscle to contract involuntarily and persistently, creating a dampening effect on sound transmission and contributing to the sensation of ear fullness. This phenomenon, known as tensor tympani syndrome , is frequently overlooked in clinical practice but represents a significant contributor to anxiety-related aural symptoms.
The stapedius muscle, which works in conjunction with the tensor tympani as part of the acoustic reflex, can also become hyperactive during periods of psychological stress. This hyperactivity creates a protective response that, while beneficial in genuinely threatening acoustic environments, becomes maladaptive when triggered by anxiety rather than actual sound threats.
Vagus nerve modulation and baroreceptor sensitivity changes
The vagus nerve, as the primary parasympathetic pathway, plays a crucial role in modulating the body’s stress response and can significantly influence inner ear function. Anxiety-induced vagal tone alterations can affect the regulation of middle ear pressure through its connections to the brainstem centres controlling Eustachian tube function. Reduced vagal tone, common in anxiety disorders, can impair the normal parasympathetic regulation of middle ear pressure equalisation.
Baroreceptors within the inner ear, responsible for detecting pressure changes, can become hypersensitive during periods of chronic anxiety. This increased sensitivity means that normal, previously unnoticed pressure fluctuations become consciously perceived as uncomfortable sensations. The heightened awareness of bodily sensations, characteristic of anxiety disorders, can amplify these normally subtle pressure variations into significant sources of distress.
Clinical manifestations of Anxiety-Related otic pressure symptoms
The presentation of anxiety-induced ear pressure varies considerably among individuals, reflecting the complex interplay between psychological factors, individual physiology, and environmental triggers. Understanding these diverse manifestations is essential for accurate diagnosis and effective treatment planning.
Subjective tinnitus and hyperacusis in generalised anxiety disorder
Patients with generalised anxiety disorder frequently report subjective tinnitus accompanied by ear pressure sensations, creating a particularly distressing symptom complex. The tinnitus often presents as a high-pitched ringing or buzzing that fluctuates in intensity with anxiety levels, suggesting a direct neurophysiological connection. This auditory phenomenon occurs when the hypervigilant state characteristic of generalised anxiety disorder causes increased attention to normally filtered auditory stimuli.
Hyperacusis, or increased sensitivity to environmental sounds, commonly coexists with anxiety-induced ear pressure. Patients describe everyday sounds as uncomfortably loud or intrusive, leading to avoidance behaviours that can further exacerbate social anxiety. The combination of pressure sensations and auditory hypersensitivity creates a cycle where environmental sounds trigger anxiety, which in turn worsens the ear symptoms, perpetuating the distress cycle.
Vestibular dysfunction patterns in panic attack episodes
During acute panic attacks, the intense activation of the sympathetic nervous system can produce vestibular symptoms including dizziness, vertigo, and ear pressure. These symptoms often occur simultaneously with the classic panic attack manifestations of rapid heartbeat, sweating, and feelings of impending doom. The vestibular component adds a particularly frightening dimension to the experience, as the sensation of imbalance can intensify fears of losing control or collapsing.
The temporal pattern of vestibular symptoms during panic attacks typically follows the overall anxiety curve, with symptoms peaking within minutes and gradually subsiding as the sympathetic response diminishes. However, some individuals experience prolonged vestibular dysfunction that persists beyond the acute episode, potentially due to sustained muscle tension or ongoing hypervigilance to bodily sensations.
Temporal bone pressure sensations during social anxiety events
Social anxiety disorder often produces distinctive ear pressure patterns that correlate with specific social situations or anticipated social encounters. Patients frequently report a sense of heaviness or pressure around the temporal bone region, accompanied by feelings of hearing impairment or sound distortion. These sensations can be particularly problematic in social situations where clear communication is essential, creating additional anxiety about potential embarrassment or social failure.
The anticipatory nature of social anxiety means that ear pressure symptoms may begin hours or even days before a stressful social event. This prolonged symptom duration reflects the sustained activation of stress response systems and highlights the importance of addressing both the psychological triggers and the physical manifestations in treatment planning.
Auricular fullness in Post-Traumatic stress disorder presentations
Individuals with post-traumatic stress disorder (PTSD) often experience ear fullness as part of their hypervigilance symptom cluster. The sensation of blocked or pressurised ears can represent the body’s attempt to modify auditory perception in response to trauma-related triggers. This mechanism may serve an adaptive function by reducing the clarity of potentially threatening sounds, but becomes maladaptive when it interferes with normal daily functioning.
The auricular symptoms in PTSD patients often show a distinct pattern of exacerbation during trauma anniversary dates or when exposed to trauma-related triggers. This temporal relationship between psychological triggers and physical symptoms provides important diagnostic information and can inform targeted treatment approaches that address both the underlying trauma and the somatic manifestations.
Differential diagnosis between Anxiety-Induced and organic ear pressure
Distinguishing between anxiety-related ear pressure and organic otological conditions presents significant clinical challenges, particularly when symptoms overlap considerably. The key lies in recognising specific patterns and characteristics that differentiate psychosomatic from pathological presentations. Anxiety-induced symptoms typically demonstrate a strong temporal correlation with stress levels and psychological triggers, whereas organic conditions usually follow more predictable pathophysiological patterns.
Organic ear pressure conditions, such as Eustachian tube dysfunction due to allergic rhinitis or acute otitis media, generally present with consistent symptoms that respond to specific medical interventions. In contrast, anxiety-related symptoms often fluctuate dramatically based on psychological state and may show paradoxical responses to traditional ear treatments. The absence of objective findings on otoscopic examination, combined with normal tympanometry results, strongly suggests a psychosomatic aetiology.
Clinical experience demonstrates that patients with anxiety-induced ear pressure often describe their symptoms in more elaborate and emotionally charged language compared to those with organic conditions, reflecting the heightened emotional significance of their somatic experience.
The response to anxiolytic interventions provides valuable diagnostic information, as anxiety-related ear symptoms typically show improvement with stress reduction techniques or anti-anxiety medications. Conversely, organic conditions require specific otological treatments and show little improvement with psychological interventions alone. A comprehensive assessment should include both otological examination and psychological evaluation to ensure accurate diagnosis and appropriate treatment planning.
Timing patterns offer crucial diagnostic clues, with anxiety-related symptoms often occurring during periods of psychological stress, late at night when anxiety levels peak, or in association with specific triggers. Organic conditions typically follow more consistent temporal patterns related to physical factors such as weather changes, allergic exposures, or infectious processes. The bilateral nature of anxiety-induced symptoms, compared to the often unilateral presentation of organic conditions, provides additional diagnostic differentiation.
Evidence-based treatment protocols for Anxiety-Associated aural symptoms
The management of anxiety-induced ear pressure requires a multi-modal approach that addresses both the underlying psychological triggers and the physical manifestations. Evidence-based treatment protocols have demonstrated significant efficacy when properly implemented and tailored to individual patient needs.
Cognitive behavioural therapy techniques for somatic anxiety management
Cognitive Behavioural Therapy (CBT) represents the gold standard for treating anxiety-related somatic symptoms, including ear pressure manifestations. The therapeutic approach focuses on identifying and modifying the cognitive distortions that amplify physical sensations and create catastrophic interpretations of benign bodily experiences. Patients learn to recognise the connection between anxious thoughts and physical symptoms, developing more balanced perspectives on their auricular sensations.
Specific CBT techniques for ear pressure include symptom monitoring , where patients track the relationship between anxiety levels and ear symptoms, and cognitive restructuring exercises that challenge catastrophic interpretations of pressure sensations. Behavioural experiments, such as deliberately inducing mild ear pressure through controlled breathing exercises, help patients recognise the benign nature of their symptoms and reduce associated fear responses.
The integration of somatic awareness techniques within CBT frameworks has shown particular promise for anxiety-related ear symptoms. These approaches teach patients to observe physical sensations without judgement, reducing the emotional reactivity that often amplifies symptom severity. Progressive muscle relaxation techniques specifically targeting the muscles around the ear and jaw region can provide direct symptomatic relief while reinforcing the connection between psychological state and physical symptoms.
SSRI efficacy in reducing psychosomatic ear pressure complaints
Selective Serotonin Reuptake Inhibitors (SSRIs) have demonstrated significant efficacy in reducing anxiety-related somatic symptoms, including ear pressure complaints. The mechanism involves the modulation of serotonergic pathways that influence both anxiety levels and somatic symptom perception. Clinical trials have shown that patients receiving SSRI treatment experience not only reduced anxiety but also decreased intensity and frequency of ear pressure episodes.
The temporal pattern of SSRI response for ear pressure symptoms typically follows the general anxiety improvement timeline, with initial benefits emerging after 2-4 weeks of consistent treatment and full therapeutic effects achieved by 8-12 weeks. Patients often report that ear pressure sensations become less intrusive and anxiety-provoking even before complete symptom resolution, suggesting that the medications affect both the physical sensations and the emotional response to them.
Specific SSRIs such as sertraline and escitalopram have shown particular effectiveness for somatic anxiety symptoms, though individual responses vary considerably. The choice of medication should consider the patient’s overall anxiety presentation, comorbid conditions, and potential side effect profiles. Regular monitoring during the initial treatment phase helps optimise dosing and identify any adverse effects that might impact treatment adherence.
Mindfulness-based stress reduction and eustachian tube function
Mindfulness-Based Stress Reduction (MBSR) techniques have emerged as powerful interventions for anxiety-related ear pressure, working through multiple physiological pathways to restore normal Eustachian tube function. The practice of mindful breathing naturally regulates the autonomic nervous system, reducing sympathetic hyperactivation that contributes to middle ear pressure imbalances. Regular mindfulness practice has been shown to improve vagal tone, which directly influences the parasympathetic regulation of Eustachian tube opening.
Specific mindfulness techniques for ear pressure include body scanning exercises that help patients develop awareness of tension patterns around the ear and jaw regions, and breathing exercises that promote gentle pressure equalisation. The non-judgemental awareness cultivated through mindfulness practice reduces the catastrophic thinking patterns that often amplify ear pressure sensations and create secondary anxiety about the symptoms.
Research has demonstrated that consistent mindfulness practice leads to measurable changes in stress hormone levels, including reduced cortisol production and improved stress resilience. These physiological changes directly impact the inflammatory processes and fluid dynamics within the middle ear, providing a scientific basis for the symptomatic improvements observed in clinical practice.
Benzodiazepine intervention for acute Anxiety-Related otic distress
Benzodiazepines can provide rapid relief for acute episodes of anxiety-related ear pressure, particularly when symptoms are severe and significantly impact daily functioning. The immediate anxiolytic effects help break the cycle of anxiety and symptom amplification, providing patients with much-needed relief during crisis periods. However, their use must be carefully managed due to the potential for tolerance and dependence.
Short-acting benzodiazepines such as lorazepam or alprazolam are typically preferred for acute intervention, with dosing tailored to the individual’s symptom severity and previous medication history. The goal is to provide sufficient relief to allow implementation of other therapeutic interventions while avoiding the development of medication dependence. Clear treatment protocols should establish specific indications for use and duration limits to prevent inappropriate long-term usage.
The integration of benzodiazepine therapy with other treatment modalities enhances overall effectiveness while minimising medication risks. Patients receiving short-term benzodiazepine treatment should simultaneously engage in CBT or other psychological interventions to develop sustainable coping strategies for future symptom episodes.
Comorbidity patterns between anxiety disorders and otological conditions
The relationship between anxiety disorders and otological conditions extends beyond simple anxiety-induced symptoms to encompass complex patterns of comorbidity that significantly impact treatment outcomes. Clinical observations reveal that individuals with pre-existing ear conditions often develop secondary anxiety disorders, while those with primary anxiety disorders may be more susceptible to developing organic ear problems due to chronic stress-related physiological changes.
Patients with Ménière’s disease, for example, demonstrate significantly higher rates of anxiety and panic disorders compared to the general population. The unpredictable nature of vertigo attacks creates anticipatory anxiety that can become as debilitating as the original otological symptoms. This secondary anxiety often perpetuates and amplifies the physical symptoms, creating a complex clinical presentation that requires integrated treatment approaches addressing both the organic ear condition and the psychological comorbidity.
Research indicates that approximately 60% of patients with chronic tinnitus develop clinically significant anxiety symptoms within the first year of symptom onset, highlighting the profound psychological impact of persistent auditory disturbances.
The presence of anxiety comorbidity in otological patients significantly
complicates treatment decisions and outcomes, as the psychological distress can amplify somatic symptom perception and interfere with objective clinical assessments. Traditional otological treatments may provide limited relief when significant anxiety components remain unaddressed, necessitating collaborative care approaches involving both ENT specialists and mental health professionals.
Chronic otitis media with effusion shows particularly strong associations with generalised anxiety disorder, especially in adult patients where childhood ear problems may have created lasting psychological associations between ear sensations and health anxiety. The persistent low-grade inflammation associated with chronic ear conditions can trigger ongoing activation of stress response systems, creating a bidirectional relationship where ear problems worsen anxiety and anxiety perpetuates ear dysfunction through inflammatory mediators and muscle tension patterns.
Acoustic trauma survivors frequently develop complex presentations combining post-traumatic stress disorder with tinnitus and hyperacusis, creating challenging clinical scenarios where psychological and auditory symptoms are inextricably linked. The sudden onset nature of acoustic trauma can create lasting associations between specific sounds and danger, leading to phonophobic behaviours that significantly impact social functioning and quality of life. Treatment approaches must address both the auditory processing changes and the trauma-related psychological responses to achieve optimal outcomes.
Age-related hearing loss (presbycusis) demonstrates interesting comorbidity patterns with late-onset anxiety disorders, particularly in individuals who have not developed effective coping strategies for gradual hearing decline. The social isolation that often accompanies hearing loss can contribute to the development of anxiety symptoms, while the anxiety can make individuals more sensitive to their hearing difficulties, creating a compounding effect that accelerates functional decline beyond what would be expected from the audiological impairment alone.
Studies examining the bidirectional relationship between anxiety and hearing disorders reveal that effective treatment of one condition often leads to spontaneous improvement in the other, emphasising the importance of comprehensive assessment and integrated treatment planning.
The temporal relationship between anxiety episodes and otological symptom exacerbations provides important insights into treatment timing and intervention strategies. Patients often report that ear symptoms worsen during periods of life stress, relationship difficulties, or work-related pressure, suggesting that stress management interventions may be as important as traditional otological treatments for long-term symptom control. This observation has led to the development of integrated treatment protocols that simultaneously address psychological stress and otological dysfunction through coordinated care approaches.