Discovering an unexpected lump on the back of your head can understandably cause concern and anxiety. While the vast majority of cranial bumps prove benign, understanding the various potential causes helps distinguish between minor conditions requiring minimal intervention and those necessitating immediate medical attention. The posterior scalp region frequently develops various types of lumps due to its rich vascular supply, dense hair follicle distribution, and susceptibility to trauma from everyday activities.
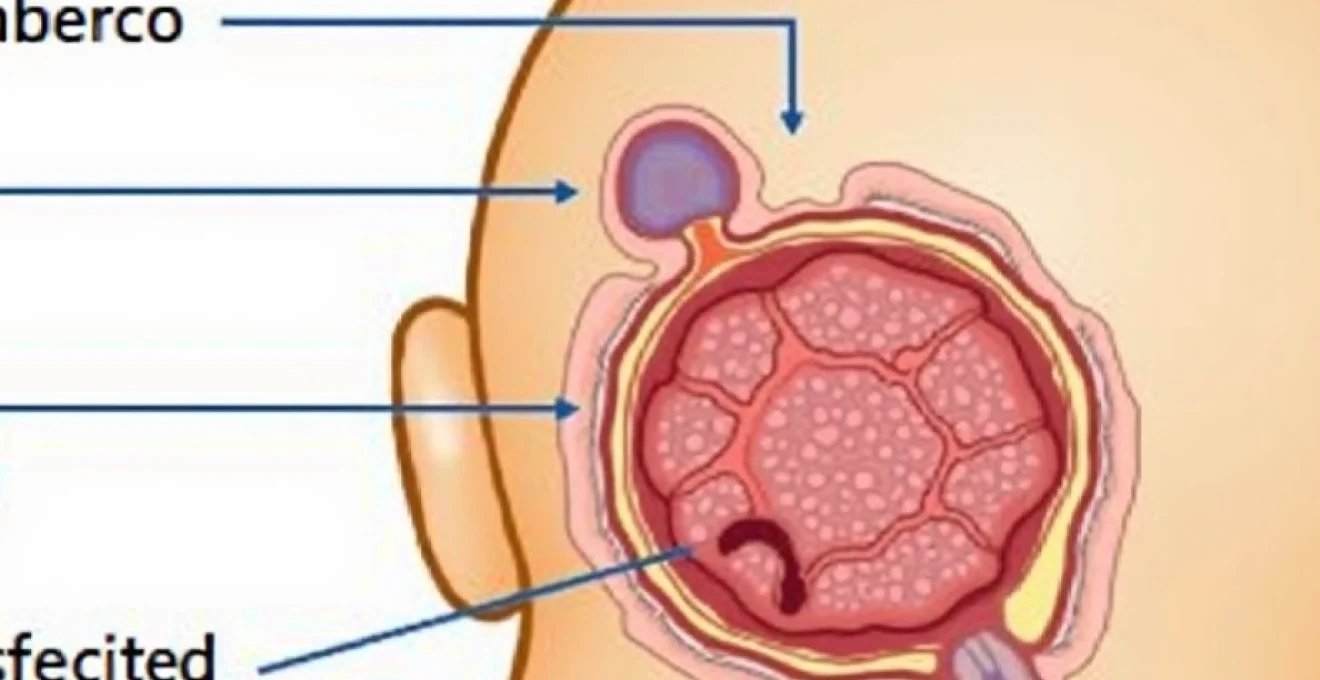
Head lumps manifest through diverse mechanisms, ranging from simple cystic formations to complex vascular malformations. The scalp’s unique anatomical structure, comprising five distinct layers, creates an environment where different pathological processes can occur at various depths. Most commonly, these lumps develop within the subcutaneous tissue or at the level of hair follicles, though deeper structures may occasionally be involved.
Sebaceous cysts and epidermoid cysts: benign epithelial growths
Epithelial cysts represent some of the most frequently encountered lumps on the posterior scalp, arising from different cellular origins yet sharing similar clinical presentations. These benign growths develop when epithelial cells become trapped beneath the skin surface, continuing to produce their characteristic substances within an enclosed space. The scalp provides an ideal environment for cyst formation due to its high concentration of hair follicles and sebaceous glands.
Keratin-filled epidermoid cyst formation and characteristics
Epidermoid cysts, often mistakenly called sebaceous cysts, originate from infundibular portions of hair follicles where keratinocytes accumulate within a keratinising squamous epithelium lining. These lesions typically present as smooth, dome-shaped nodules ranging from several millimetres to several centimetres in diameter. The cyst wall consists of stratified squamous epithelium that continuously sheds keratin debris into the central cavity, creating the characteristic cheese-like consistency that patients sometimes observe if the cyst ruptures spontaneously.
The slow growth pattern of epidermoid cysts makes them easily distinguishable from rapidly expanding inflammatory conditions. Most patients report gradual enlargement over months or years, with occasional periods of inflammation when bacterial contamination occurs. A central punctum, appearing as a small dark spot on the cyst surface, often provides a definitive diagnostic clue and represents the original follicular opening where epithelial invagination initially occurred.
Pilar cysts: trichilemmal keratinisation patterns
Pilar cysts, also termed trichilemmal cysts, demonstrate a distinct predilection for scalp locations, accounting for approximately 90% of all scalp cysts encountered in clinical practice. These lesions arise from the outer root sheath of hair follicles and exhibit trichilemmal keratinisation, a process characterised by abrupt transition from nucleated cells to compact keratin without an intervening granular layer. This unique keratinisation pattern distinguishes pilar cysts histologically from their epidermoid counterparts.
Genetic factors play a significant role in pilar cyst development, with autosomal dominant inheritance patterns observed in many affected families. Multiple pilar cysts frequently occur simultaneously, particularly in middle-aged women, and these lesions typically remain asymptomatic unless secondary inflammation develops. The cyst contents appear more homogeneous than epidermoid cyst material, lacking the laminated keratin structure seen in the latter condition.
Sebaceous adenoma and hyperplasia differentiation
True sebaceous proliferations occur less frequently on the scalp but merit consideration in the differential diagnosis of head lumps. Sebaceous adenomas represent benign neoplasms composed of mature sebaceous lobules with varying degrees of cellular maturation, while sebaceous hyperplasia manifests as yellowish papules containing enlarged sebaceous glands surrounding dilated central pores. These conditions typically affect older adults and may occasionally be associated with internal malignancies, particularly in patients with multiple lesions.
Clinical differentiation between sebaceous proliferations and conventional cysts relies on careful examination of surface characteristics and growth patterns. Sebaceous lesions often display a more yellowish coloration and softer consistency compared to keratin-filled cysts, reflecting their lipid-rich composition. The presence of central umbilication in sebaceous hyperplasia provides an additional diagnostic feature that helps distinguish these lesions from other scalp bumps.
Dermoid cyst embryological development anomalies
Dermoid cysts represent developmental anomalies resulting from ectodermal tissue entrapment during embryonic neural tube closure. These lesions contain mature skin appendages, including hair follicles, sebaceous glands, and occasionally teeth or bone fragments, creating complex internal architecture. Posterior scalp dermoid cysts typically present in young children as slowly enlarging masses that may demonstrate deeper extension toward intracranial structures.
The clinical significance of dermoid cysts extends beyond their benign nature due to potential intracranial connections that occur in approximately 20% of cases. Imaging studies become essential for surgical planning, as inadvertent rupture of intracranially connected dermoids can precipitate severe inflammatory reactions. These lesions require complete surgical excision to prevent recurrence, and careful preoperative evaluation helps identify patients requiring neurosurgical consultation.
Lipomatous lesions and subcutaneous fat proliferation
Adipose tissue proliferations encompass various benign conditions characterised by abnormal fat accumulation within subcutaneous spaces. While lipomas represent the most common soft tissue tumours encountered throughout the body, their occurrence on the scalp remains relatively uncommon compared to other anatomical sites. The unique biomechanical properties of scalp tissue, including its rich vascular supply and firm attachment to underlying structures, influence lipomatous lesion development and clinical behaviour.
Superficial lipoma: adipocyte encapsulation mechanisms
Superficial lipomas develop within subcutaneous tissue planes, presenting as soft, mobile masses with characteristic doughy consistency upon palpation. These lesions consist of mature adipocytes surrounded by thin fibrous capsules that facilitate their surgical removal. The mobility of superficial lipomas distinguishes them from deeper-seated masses and inflammatory conditions, as gentle pressure typically allows these lesions to slide freely beneath the skin surface.
Growth patterns of scalp lipomas tend to be extremely slow, with most lesions remaining stable for years without significant size changes. Rapid enlargement suggests possible malignant transformation to liposarcoma, though this complication occurs exceedingly rarely in superficial locations. Pain development within previously asymptomatic lipomas may indicate internal bleeding, infection, or pressure effects on surrounding structures, warranting prompt medical evaluation.
Angiolipoma vascular component analysis
Angiolipomas represent a distinct lipomatous variant characterised by prominent vascular proliferation within adipose tissue matrices. These lesions typically demonstrate greater tenderness compared to conventional lipomas due to their rich blood supply and potential for internal microthrombi formation. The vascular component becomes particularly evident during histopathological examination, revealing numerous small vessels intimately admixed with mature fat cells.
Clinical recognition of angiolipomas relies on their characteristic pain sensitivity, particularly in response to cold temperatures or mechanical pressure. Multiple angiolipomas may occur simultaneously, creating diagnostic confusion with other conditions causing multiple scalp nodules. The enhanced vascularity of these lesions necessitates careful surgical technique during excision to minimise bleeding complications and ensure complete removal.
Hibernoma brown fat tissue characteristics
Hibernomas represent exceptionally rare benign tumours composed of brown adipose tissue, more commonly encountered in infants and young adults. These lesions derive from persistent embryonic brown fat and typically occur in characteristic anatomical distributions, including the posterior neck region where they may extend onto the posterior scalp. The cellular composition of hibernomas includes multivacuolated adipocytes with abundant mitochondria, giving these tumours their characteristic brownish coloration.
The clinical significance of hibernomas relates to their potential for significant size and their tendency to occur in locations where complete surgical excision may prove challenging. Imaging studies reveal characteristic features including heterogeneous signal intensity and prominent vascular flow, helping differentiate these lesions from conventional lipomas or other soft tissue masses.
Spindle cell lipoma histopathological features
Spindle cell lipomas demonstrate unique histological characteristics combining mature adipose tissue with fascicles of bland spindle cells and prominent collagen bundles. These lesions typically affect older men and show a predilection for the posterior neck and shoulder regions, occasionally extending onto the posterior scalp. The spindle cell component may create diagnostic uncertainty, necessitating expert histopathological evaluation to exclude malignant possibilities.
The fibrous component within spindle cell lipomas can create firmer consistency compared to conventional lipomas, potentially leading to clinical confusion with other fibrous proliferations. Complete surgical excision remains the treatment of choice, with excellent prognosis following adequate removal. Recurrence rates remain low provided that complete excision achieves negative surgical margins.
Inflammatory and infectious nodular conditions
Infectious and inflammatory processes affecting the posterior scalp create various nodular lesions that may initially concern patients due to their rapid onset and associated symptoms. The scalp’s dense hair follicle population provides numerous potential sites for bacterial colonisation and subsequent infection development. Understanding the pathogenesis and clinical presentation of these conditions helps differentiate them from neoplastic processes and guides appropriate therapeutic interventions.
Folliculitis decalvans scalp involvement patterns
Folliculitis decalvans represents a chronic inflammatory condition characterised by recurrent episodes of deep follicular infection leading to progressive scarring alopecia. This condition typically affects the vertex and posterior scalp regions, creating inflammatory nodules that eventually evolve into permanent hair loss areas. The pathogenesis involves persistent Staphylococcus aureus colonisation within hair follicles, triggering intense inflammatory responses that destroy follicular structures.
Clinical presentation includes tender, erythematous nodules surrounding affected hair follicles, often accompanied by pustule formation and crusting. The chronic nature of this condition distinguishes it from acute infectious processes, as patients typically report recurring episodes over months or years. Bacterial culture and sensitivity testing guide antibiotic selection, though long-term suppressive therapy may be necessary to prevent disease progression and additional scarring.
Carbuncle and furuncle staphylococcal pathogenesis
Carbuncles and furuncles represent acute bacterial infections of hair follicles and surrounding tissues, typically caused by Staphylococcus aureus strains. Furuncles involve single follicular units, while carbuncles encompass multiple adjacent follicles, creating larger, more extensive inflammatory masses. The posterior scalp location provides an ideal environment for these infections due to increased friction from headrests, pillows, and hair manipulation.
The inflammatory response in carbuncles creates significant tissue oedema and erythema, often accompanied by systemic symptoms including fever and malaise. Spontaneous drainage commonly occurs through multiple surface points, releasing purulent material and providing symptomatic relief. However, premature incision may lead to incomplete drainage and recurrence, making appropriate timing of surgical intervention crucial for optimal outcomes.
Pilonidal sinus tract formation mechanisms
While pilonidal sinuses typically occur in sacrococcygeal regions, similar mechanisms can create analogous lesions on the posterior scalp, particularly in individuals with coarse hair and poor hygiene practices. These lesions develop when shed hairs penetrate skin surfaces and migrate into subcutaneous tissues, creating foreign body reactions and chronic sinus tract formation. The mechanical action of head movement facilitates hair penetration and subsequent inflammatory responses.
Clinical manifestations include recurrent episodes of swelling, drainage, and discomfort in affected areas. The presence of protruding hair shafts from sinus openings provides pathognomonic evidence of the underlying condition. Treatment requires complete excision of sinus tracts and surrounding inflammatory tissue to prevent recurrence, as incomplete removal invariably leads to persistent symptoms.
Tricholemmal proliferating cyst malignant transformation risk
Proliferating tricholemmal cysts represent a unique variant of pilar cysts characterised by increased cellular proliferation and potential for malignant transformation. These lesions typically occur in elderly patients and demonstrate more aggressive growth patterns compared to conventional pilar cysts. The proliferative component creates irregular internal architecture that may be mistaken for malignancy during initial evaluation.
The risk of malignant transformation to tricholemmal carcinoma, though low, necessitates complete histopathological evaluation of all excised specimens. Clinical features suggesting malignant potential include rapid growth, irregular surface characteristics, and ulceration. Long-term follow-up becomes essential for patients with proliferating tricholemmal cysts due to their potential for local recurrence and malignant progression.
Trauma-related haematomas and Post-Injury sequelae
Traumatic injuries to the posterior scalp frequently result in haematoma formation, creating palpable lumps that may persist for extended periods following the initial injury. The scalp’s rich vascular supply predisposes this region to significant bleeding following even minor trauma, as blood accumulates within tissue planes creating characteristic fluctuant masses. Understanding the natural history of post-traumatic scalp lumps helps distinguish between benign healing responses and complications requiring medical intervention.
Scalp haematomas typically develop immediately following trauma, though delayed presentations may occur when initial bleeding remains minimal. The classic “goose egg” appearance results from blood accumulation between the periosteum and overlying soft tissues, creating a well-defined, fluctuant mass. Most traumatic scalp haematomas resolve spontaneously over several weeks through reabsorption processes, though larger collections may require drainage to prevent complications such as infection or calcification.
Subgaleal haematomas represent more extensive bleeding patterns involving the loose connective tissue plane beneath the galea aponeurotica. These lesions can extend across large scalp areas due to the absence of anatomical barriers within this tissue plane. The clinical significance of subgaleal haematomas relates to their potential for significant blood loss, particularly in paediatric patients where these collections may contribute to haemodynamic instability.
Chronic organised haematomas may persist for months following the initial traumatic event, creating firm masses that can be confused with neoplastic processes. These lesions undergo gradual organisation through fibrin deposition and cellular infiltration, eventually forming encapsulated collections that may require surgical removal. Calcification within chronic haematomas creates additional diagnostic complexity, as these deposits may be palpable as hard lumps that concern patients and clinicians alike.
Early recognition and appropriate management of traumatic scalp haematomas significantly reduces the risk of long-term complications and ensures optimal cosmetic outcomes for affected patients.
Vascular malformations and haemangiomatous lesions
Vascular anomalies affecting the posterior scalp encompass both proliferative haemangiomas and structural vascular malformations, each demonstrating distinct clinical behaviours and treatment requirements. These lesions may present as soft, compressible masses with varying degrees of surface discoloration, depending on their depth and vascular composition. The scalp’s abundant blood supply creates an environment where vascular anomalies can achieve considerable size and complexity.
Infantile haemangiomas typically undergo characteristic growth phases, including rapid proliferation during the first year of life followed by gradual involution over subsequent years. Scalp haemangiomas may create significant cosmetic concerns for parents, though most lesions resolve spontaneously without intervention. However, large or rapidly growing haemangiomas may require treatment to prevent complications such as ulceration, bleeding, or functional impairment.
Arteriovenous malformations represent high-flow vascular anomalies with direct arterial-to-venous connections bypassing normal capillary beds. These lesions may present as pulsatile masses with associated bruits audible on auscultation. The high-flow nature of arteriovenous malformations creates potential for significant complications including bleeding, heart failure, and neurological symptoms if intracranial extension occurs.
Venous malformations appear as soft, compressible masses that enlarge with dependent positioning or Valsalva manoeuvres. These low-flow lesions typically demonstrate bluish discoloration when located superficially and may cause discomfort due to thrombosis or expansion. Unlike haemangiomas, venous malformations persist throughout life without spontaneous resolution, often requiring intervention for symptomatic relief or cosmetic improvement.
Lymphatic malformations may also occur in scalp locations, presenting as cystic masses with varying consistency depending on their internal structure. Macrocystic lymphatic malformations appear as large, fluctuant masses, while microcystic variants demonstrate firmer consistency due to their intricate internal
architecture. These lesions may undergo secondary infection or hemorrhage, creating acute enlargement and discomfort that requires prompt medical attention.
When to seek immediate medical evaluation: red flag symptoms
While most posterior scalp lumps represent benign conditions requiring minimal intervention, certain clinical features warrant immediate medical evaluation to exclude serious underlying pathology. Understanding these warning signs empowers patients to seek appropriate care and helps healthcare providers prioritise urgent cases requiring expedited assessment. The combination of clinical presentation, growth characteristics, and associated symptoms provides crucial information for risk stratification and management planning.
Rapid growth represents one of the most concerning features in any scalp lump, as malignant processes typically demonstrate accelerated expansion compared to benign conditions. Lumps that double in size within weeks or demonstrate irregular growth patterns require immediate evaluation to exclude aggressive neoplasms or severe infections. Similarly, changes in surface characteristics including ulceration, bleeding, or colour variation may indicate malignant transformation or advanced infectious processes necessitating urgent intervention.
Neurological symptoms accompanying scalp lumps raise significant concerns about potential intracranial involvement or compression effects on underlying structures. Headaches that worsen progressively, visual disturbances, seizures, or focal neurological deficits may indicate deeper extension of scalp lesions or associated intracranial pathology. These symptoms require emergency evaluation including advanced imaging studies to assess for brain involvement or increased intracranial pressure.
Systemic symptoms such as fever, night sweats, unexplained weight loss, or general malaise occurring in conjunction with scalp lumps may suggest infectious processes, inflammatory conditions, or malignant disease requiring comprehensive evaluation. The presence of multiple lumps throughout the body, particularly in lymph node regions, raises concerns about systemic lymphoproliferative disorders or metastatic disease that demands immediate investigation.
Pain characteristics provide additional diagnostic clues, as sudden onset of severe pain within previously asymptomatic lumps may indicate complications such as infection, bleeding, or malignant transformation requiring urgent medical attention.
Certain patient populations face elevated risks for serious scalp pathology and warrant lower thresholds for medical evaluation. Immunocompromised individuals, including those receiving chemotherapy, chronic steroid therapy, or living with HIV infection, demonstrate increased susceptibility to aggressive infections and unusual malignancies. Similarly, patients with previous cancer diagnoses require careful evaluation of new scalp lumps to exclude metastatic disease or treatment-related complications.
The inability to move underlying scalp tissue or fixation of lumps to deeper structures suggests potential involvement of skull bone, muscle, or intracranial contents. These findings necessitate immediate evaluation including imaging studies to assess the extent of involvement and plan appropriate treatment strategies. Fixed lumps often require multidisciplinary management involving neurosurgical consultation and specialised treatment approaches.
Changes in previously stable lumps demand prompt medical attention, as transformation of long-standing benign lesions may indicate malignant progression or secondary complications. Patients should monitor existing scalp lumps for changes in size, consistency, mobility, or surface characteristics, seeking evaluation when any significant alterations occur. The development of satellite lesions around existing lumps may suggest aggressive growth patterns or infectious spread requiring immediate intervention.
Finally, any scalp lump accompanied by neurological deficits, persistent drainage despite treatment, or failure to respond to appropriate therapy warrants immediate medical evaluation. These presentations suggest either misdiagnosis of the underlying condition or development of complications requiring advanced treatment approaches. Early recognition and prompt treatment of concerning scalp lumps significantly improve outcomes and prevent potential complications that may arise from delayed intervention.