The intersection of urological health and reproductive function raises intriguing questions that many patients hesitate to discuss openly with their healthcare providers. Recent research has begun to explore the fascinating relationship between sexual activity and kidney stone passage, challenging traditional assumptions about treatment approaches. While conventional wisdom focuses on hydration, medication, and surgical interventions for nephrolithiasis management, emerging evidence suggests that physiological responses during ejaculation may indeed facilitate stone expulsion in specific circumstances.
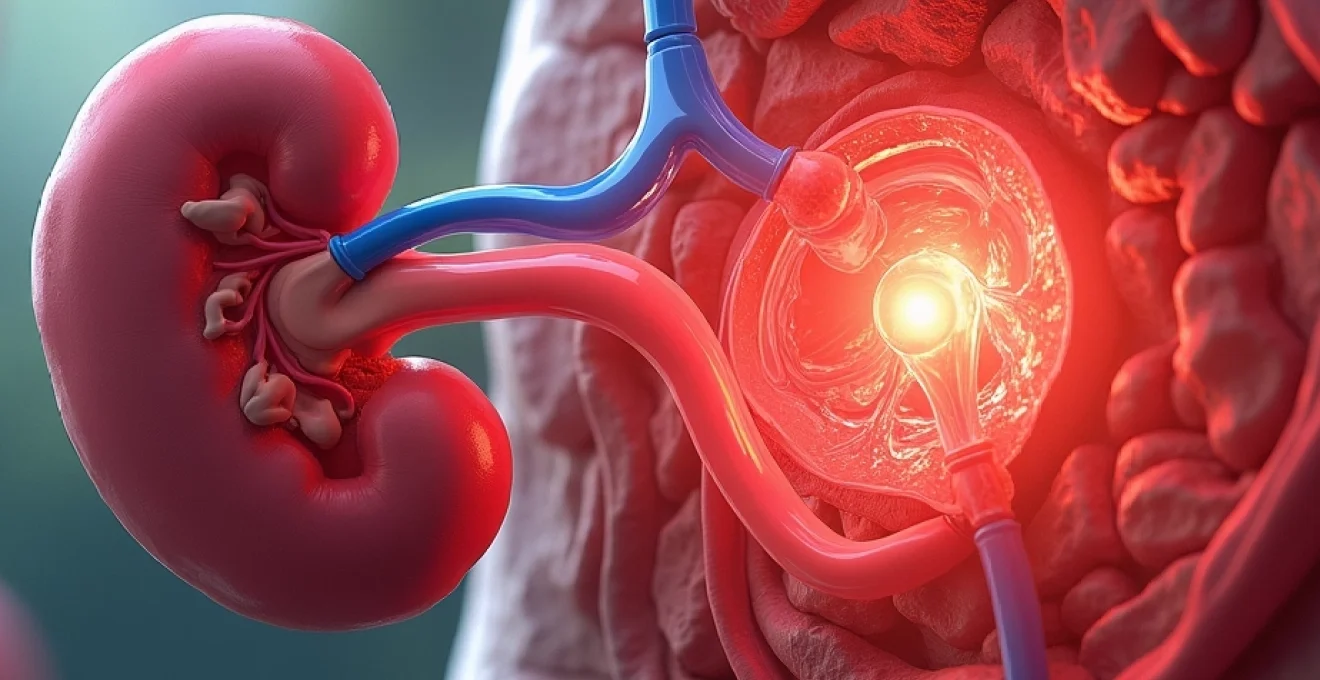
Understanding the anatomical connections between urinary and reproductive systems becomes crucial when examining this phenomenon. The shared pathways and overlapping muscular mechanisms create opportunities for stones to traverse unexpected routes during moments of heightened physiological activity. This topic deserves careful examination from both clinical and patient perspectives, particularly given the potential implications for treatment protocols and patient counselling.
Anatomical pathways: urinary and reproductive system intersections
The male reproductive and urinary systems share critical anatomical structures that create potential pathways for kidney stone migration during ejaculatory events. The urethra serves as a common conduit for both urine and seminal fluid, extending from the bladder neck through the prostate, corpus spongiosum, and glans penis. This shared pathway represents the primary route through which a kidney stone might theoretically exit during ejaculation, though the mechanics involve complex physiological processes.
The positioning of reproductive organs relative to urinary structures creates unique opportunities for stone movement. During sexual arousal and ejaculation, significant changes occur in pelvic blood flow, muscle contractions, and internal pressure dynamics. These changes can influence the behaviour of stones already positioned within the lower urinary tract, potentially facilitating their expulsion through coordinated muscular contractions and increased hydraulic pressure.
Prostatic urethra and ejaculatory duct convergence points
The prostatic urethra represents a critical anatomical junction where ejaculatory ducts merge with the urinary pathway. This convergence point, located at the verumontanum, creates a complex environment where stones measuring less than 4-6 millimetres might become temporarily lodged. During ejaculation, the coordinated contractions of periurethral muscles and the sudden influx of seminal fluid can generate sufficient force to dislodge small calculi from this location.
The ejaculatory ducts themselves, measuring approximately 2 centimetres in length, enter the prostatic urethra at acute angles. This anatomical arrangement means that retrograde pressure from ejaculatory contractions can create hydraulic forces capable of mobilising stones positioned within the distal prostatic urethra. The timing and coordination of these muscular contractions become crucial factors in determining whether stone expulsion occurs during climax.
Seminal vesicle positioning relative to ureter pathways
Seminal vesicles, located posterior to the bladder base, maintain close anatomical proximity to the terminal portions of both ureters. This positioning creates potential for stones descending through the ureterovesical junction to be influenced by seminal vesicle contractions during ejaculation. The muscular walls of seminal vesicles contract forcefully during climax, generating pressures that can exceed 40 mmHg in healthy individuals.
The anatomical relationship between seminal vesicles and the trigone region of the bladder becomes particularly relevant when considering stone migration patterns. Stones measuring 2-4 millimetres that have successfully navigated the ureter but remain within the intramural portion may be subject to expulsive forces generated by coordinated contractions of both seminal vesicles and detrusor muscle fibres during orgasmic response.
Bladder neck sphincter mechanism during ejaculatory response
The bladder neck sphincter mechanism undergoes dramatic changes during ejaculatory response, with sympathetic nervous system activation causing intense contraction of smooth muscle fibres. This contraction serves dual purposes: preventing retrograde ejaculation into the bladder while simultaneously creating positive pressure within the proximal urethra. For stones positioned at the bladder neck or within the proximal prostatic urethra, these pressure changes can provide the necessary force for antegrade expulsion.
Alpha-adrenergic stimulation during climax causes maximal contraction of bladder neck smooth muscle, generating pressures that can exceed those achieved through normal voiding mechanisms. This enhanced pressure differential, combined with coordinated rhythmic contractions of bulbospongiosus and ischiocavernosus muscles , creates optimal conditions for small stone expulsion through the urethral pathway.
Retrograde ejaculation and urinary stone migration potential
Retrograde ejaculation, while generally considered a dysfunction, presents an interesting scenario for potential stone migration in the opposite direction. When bladder neck closure fails during ejaculation, seminal fluid travels retrograde into the bladder, potentially carrying small urethral stones with it. This reverse migration could theoretically move stones from the urethra back into the bladder, where they might be more easily expelled during subsequent urination.
The phenomenon of retrograde ejaculation occurs in approximately 0.3-2% of fertile men but increases significantly in those with diabetes, neurological conditions, or following certain medical procedures. In these cases, the altered pressure dynamics and flow patterns could influence stone behaviour differently than in normal antegrade ejaculation, potentially creating alternative pathways for calculi movement within the urinary system.
Nephrolithiasis physiology and stone composition analysis
The likelihood of stone expulsion during ejaculation depends heavily on the physical characteristics of the calculus itself, including size, composition, surface texture, and overall structural integrity. Different stone types exhibit varying degrees of friability and response to hydraulic forces, making composition analysis crucial for predicting the success of spontaneous passage through any mechanism. Understanding these material properties helps clinicians assess whether sexual activity might facilitate stone expulsion in individual cases.
Stone formation occurs through complex crystallisation processes involving supersaturated urine and inadequate inhibitory factors. The resulting calculi range from microscopic crystals to large staghorn formations, with the vast majority measuring between 2-8 millimetres in diameter. Only stones within specific size parameters possess realistic potential for expulsion during ejaculatory events, making accurate measurement and characterisation essential for appropriate patient counselling.
Calcium oxalate crystal formation and size distribution
Calcium oxalate stones represent approximately 75-80% of all renal calculi, displaying characteristic crystalline structures that influence their passage potential. These stones typically form through calcium and oxalate supersaturation in urine, creating monohydrate or dihydrate crystal formations with distinct physical properties. Calcium oxalate monohydrate stones appear darker and more compact, while dihydrate varieties tend to be lighter coloured and more friable.
The surface characteristics of calcium oxalate stones significantly impact their likelihood of spontaneous passage. Smooth, rounded stones measuring less than 4 millimetres demonstrate higher passage rates through narrow urethral segments, while irregular or spiculated surfaces create increased friction and reduced mobility. Ejaculatory forces may prove more effective against smaller, smoother calcium oxalate formations than larger or more irregular specimens.
Uric acid stone characteristics and dissolution properties
Uric acid stones, comprising 5-10% of all kidney stones, exhibit unique properties that may influence their behaviour during ejaculatory expulsion attempts. These radiolucent stones form in acidic urine environments and typically appear smooth and yellow-orange in colour. Their relative softness compared to calcium-based stones makes them more susceptible to mechanical forces generated during sexual climax.
The dissolution properties of uric acid stones create additional considerations for expulsion dynamics. Unlike calcium oxalate formations, uric acid calculi can undergo partial dissolution in alkaline environments, potentially reducing their effective size during transit through the urinary system. This size reduction might facilitate passage through anatomical restrictions that would otherwise prevent successful stone expulsion during ejaculation.
Struvite and cystine stone physical parameters
Struvite stones, also known as infection stones, form in alkaline urine and can achieve considerable size due to their rapid growth patterns. These magnesium ammonium phosphate formations typically develop smooth surfaces but can reach dimensions that make spontaneous passage unlikely through conventional mechanisms. The large size potential of struvite stones generally precludes their expulsion during ejaculatory events.
Cystine stones represent the hardest naturally occurring kidney stone variety, formed through inherited metabolic disorders affecting amino acid transport. These stones exhibit characteristic hexagonal crystal structures and yellow coloration, with exceptional resistance to both mechanical forces and chemical dissolution. The extraordinary hardness of cystine stones makes them particularly unlikely candidates for expulsion through ejaculatory mechanisms, regardless of size considerations.
Stone surface texture impact on urethral transit
Surface texture plays a crucial role in determining whether stones can successfully navigate the urethral pathway during ejaculation. Smooth, polished stone surfaces encounter minimal friction resistance, allowing for easier passage through anatomical constrictions such as the external urethral meatus. Conversely, rough or spiculated surfaces create increased drag and potential for tissue trauma during transit attempts.
The relationship between surface texture and successful stone expulsion becomes particularly important when considering the limited diameter of the penile urethra, which measures approximately 5-6 millimetres at its narrowest point. Stones with irregular surfaces may become lodged within the corpus spongiosum, creating painful obstruction that requires immediate medical intervention. Understanding these textural factors helps predict which stones might safely pass during ejaculatory events.
Millimetre classification system for passable calculi
Urological literature consistently demonstrates that stone size represents the most critical factor in predicting spontaneous passage rates through the urinary system. The millimetre classification system provides standardised categories for assessing passage likelihood, with stones measuring less than 4 millimetres showing passage rates exceeding 85% through conventional mechanisms. This size threshold becomes even more critical when considering passage during ejaculatory events.
Stones measuring 4-6 millimetres demonstrate intermediate passage rates of approximately 50-70%, depending on location and patient factors. Beyond 6 millimetres, spontaneous passage rates drop dramatically to less than 20%, making ejaculatory expulsion highly unlikely for calculi in this size range. These statistical parameters provide essential guidance for clinicians counselling patients about realistic expectations regarding sexual activity as a potential stone management strategy.
Documented case studies: stone expulsion during sexual activity
Clinical literature contains scattered reports of kidney stone expulsion during sexual climax, though comprehensive documentation remains limited due to patient reluctance to report such incidents and physician hesitation to inquire about sexual activity in urological contexts. These case reports provide valuable insights into the circumstances surrounding successful stone expulsion during ejaculation, highlighting common factors such as stone size, anatomical positioning, and patient characteristics that favour positive outcomes.
A review of available case documentation reveals that most successful expulsions involve stones measuring between 2-5 millimetres that had already progressed to the distal ureter or proximal urethra. The timing of sexual activity relative to stone positioning appears crucial, with optimal results occurring when calculi have descended beyond the ureterovesical junction but remain proximal to the penile urethra. Patient reports consistently describe immediate relief from obstructive symptoms following successful stone expulsion during climax.
Documented cases also reveal important safety considerations, including instances where attempted passage resulted in stone impaction within the urethra, requiring emergency urological intervention. These complications underscore the importance of appropriate patient selection and medical oversight when discussing sexual activity as a potential adjunctive treatment for kidney stones. The medical literature emphasises that such approaches should complement, rather than replace, established therapeutic protocols.
Recent studies suggest that sexual intercourse 3-4 times weekly may facilitate spontaneous passage of small distal ureteral stones, with success rates comparable to certain pharmaceutical interventions.
Urethral transit mechanics and ejaculatory force dynamics
The mechanics of urethral transit during ejaculation involve complex interactions between hydraulic pressure, muscular contractions, and anatomical constraints that determine whether successful stone expulsion occurs. Peak ejaculatory pressures can reach 200-400 mmHg within the prostatic urethra, generating forces sufficient to propel objects through the 15-20 centimetre urethral pathway. However, these forces must overcome both gravitational effects and frictional resistance created by stone-urethral wall interactions.
The sequential nature of ejaculatory contractions creates pulsatile pressure waves that may prove more effective than sustained pressure for stone mobilisation. Initial contractions of the bulbospongiosus muscle occur at 0.8-second intervals, followed by progressively weaker contractions as the climactic response subsides. This rhythmic pattern can provide repeated attempts at stone displacement, increasing the likelihood of successful expulsion compared to single-force applications.
Urethral diameter variations significantly influence stone transit success, with the external meatus representing the narrowest point at approximately 5-6 millimetres in healthy individuals. The navicular fossa and membranous urethra present additional constriction points that can impede stone passage despite adequate propulsive forces. Anatomical variations in urethral calibre between individuals create significant differences in stone passage potential, making generalised predictions difficult without individual assessment.
The viscoelastic properties of ejaculatory fluid contribute to stone transit mechanics by reducing friction and providing lubrication during passage attempts. Seminal fluid viscosity, influenced by factors such as abstinence duration and overall reproductive health, can affect the efficiency of stone transport through urethral segments. Higher fluid volumes and optimal viscosity characteristics generally favour successful stone expulsion when adequate propulsive forces are present.
Medical risk assessment and urological emergency protocols
Medical risk assessment for patients considering sexual activity as an adjunctive stone management strategy requires careful evaluation of multiple factors including stone characteristics, patient anatomy, and potential complications. Primary concerns include stone impaction within the urethra, trauma to delicate urethral tissues, and the possibility of incomplete passage leading to obstructive symptoms. Healthcare providers must balance the potential benefits of natural expulsion mechanisms against these significant risks.
Emergency protocols for stone-related complications during sexual activity should be established before patients attempt such interventions. Immediate medical attention becomes necessary if patients experience severe pain, inability to void, visible haematuria, or signs of urethral injury following attempted sexual expulsion. Emergency departments must be prepared to address these presentations with appropriate diagnostic imaging and urological consultation when indicated.
Patient selection criteria for considering sexual activity as a potential stone management approach should include stone size limitations (typically less than 4-5 millimetres), distal ureteral or bladder positioning confirmed by imaging, absence of active infection, and normal urethral anatomy. Patients with urethral strictures, previous urological surgery, or bleeding disorders represent relative contraindications for this approach. Comprehensive informed consent discussions must address both potential benefits and significant risks associated with such interventions.
Long-term follow-up protocols should monitor for complications such as urethral scarring, erectile dysfunction, or psychological impacts related to stone expulsion attempts during sexual activity. Some patients may develop anxiety or performance concerns related to associating sexual activity with medical treatment, requiring appropriate counselling and support. Healthcare providers must remain sensitive to these psychological dimensions while maintaining focus on optimal clinical outcomes.
Clinical differentiation between haematospermia and stone passage
Distinguishing between haematospermia (blood in semen) caused by stone passage and other potential aetiologies requires careful clinical assessment and appropriate diagnostic testing. Stone-related haematospermia typically presents as bright red blood mixed throughout the ejaculate, often accompanied by sudden onset of symptoms coinciding with sexual climax. Patients frequently report immediate relief from pre-existing urinary symptoms following episodes of bloody ejaculation associated with stone expulsion.
The temporal relationship between symptoms and stone passage provides important diagnostic clues, with stone-related haematospermia typically resolving completely after successful calculus expulsion. Persistent or recurrent bloody ejaculation following suspected stone passage warrants further investigation to exclude other pathology such as prostatitis, seminal vesicle abnormalities, or neoplastic processes. Microscopic urinalysis following stone expulsion episodes often reveals transient haematuria that gradually resolves over 24-48 hours.
Imaging confirmation of stone passage can be challenging, as successful expulsion eliminates the target lesion from subsequent studies. Comparison of pre- and post-event imaging studies provides the most reliable confirmation of successful stone passage, though this approach requires fortunate timing of diagnostic studies. Patient reports of recovering visible stone fragments from ejaculate provide definitive confirmation when such specimens are available for analysis.
Associated symptoms during stone passage episodes include sharp, shooting pains along the penile shaft, temporary urethral burning, and occasionally visible stone fragments within the ejaculate. These symptoms typically resolve rapidly following successful expulsion, contrasting with the persistent discomfort associated with other causes of haematospermia. Healthcare
providers must distinguish between these characteristic patterns and other urological conditions to provide appropriate patient management and follow-up care.
Diagnostic protocols for suspected stone-related haematospermia should include comprehensive history taking focusing on recent stone episodes, pain patterns, and associated urinary symptoms. Physical examination may reveal tenderness along the penile shaft or at the external meatus, particularly if recent stone passage has occurred. Laboratory evaluation should encompass complete urinalysis, semen analysis when feasible, and consideration of prostatic-specific antigen levels if indicated by clinical presentation.
The psychological impact of experiencing haematospermia during sexual activity cannot be overlooked, as many patients develop significant anxiety about future sexual encounters following such episodes. Reassurance regarding the benign nature of stone-related haematospermia becomes crucial for maintaining healthy sexual function and preventing long-term psychological complications. Healthcare providers must address these concerns proactively while ensuring appropriate medical follow-up for any persistent or concerning symptoms.
Documentation of stone passage events through sexual activity contributes valuable information to the growing body of literature on this phenomenon. Patients should be encouraged to report such occurrences to their healthcare providers, including details about stone recovery, symptom resolution, and any complications experienced. This information helps refine clinical understanding of the conditions under which sexual activity may serve as an effective adjunctive treatment for small kidney stones.
Follow-up imaging studies should be considered 2-4 weeks following suspected stone passage to confirm complete expulsion and assess for any retained fragments. Persistent symptoms or imaging evidence of incomplete stone clearance may necessitate conventional urological interventions despite apparent passage during sexual activity. The integration of patient-reported outcomes with objective imaging findings provides the most comprehensive assessment of treatment success in these unique clinical scenarios.
Understanding the complex interplay between reproductive physiology and urological health opens new avenues for patient counselling and treatment planning. While sexual activity should never replace established medical treatments for kidney stones, the evidence suggests it may serve as a valuable adjunctive approach for appropriately selected patients with small calculi in favourable anatomical positions.
The phenomenon of kidney stone expulsion during ejaculation represents a fascinating intersection of human anatomy, physiology, and reproductive health. As research continues to explore these connections, healthcare providers must remain open to discussing all potential treatment modalities with their patients, including those that challenge conventional therapeutic approaches. The key lies in careful patient selection, comprehensive risk assessment, and ongoing medical supervision to ensure optimal outcomes while minimizing potential complications.